Dr Senthil Velan
MBBS, MRCS(UK) FRCS (Tr &Ortho), FEBOT(France), Fellow European Board Orthopaedics and Trauma.,
D Ortho,Dip SICOT(Honk Kong).
Consultant Orthopaedic Surgeon
Apollo Hospitals Ayanambakkam , Chennai, India
For appointments and queries contact us on Ph 9566222533/ nexusortho@yahoo.com
Shoulder dislocation and instability.
What is it?
The shoulder joint is a ball and socket joint. The round end of the upper arm bone (humerus) fits into the shallow socket (glenoid) on the shoulder blade (scapula) much like a golf ball rests on a tee. The anatomy of the shoulder joint makes it the most mobile joint in the body.
While this gives us the ability to move it in many directions it also makes it an easy joint to dislocate. A complete dislocation means that the ball (humeral head) has come all the way out of the socket. When the ball comes out of the socket incompletely, it is called a partial dislocation or subluxation. When the shoulder dislocates or subluxes repeatedly it is known as shoulder instability. The shoulder joint can dislocate forward, backward or downward. The most common type is when the shoulder slips forward (anterior).
What is its cause?
A ring of cartilage surrounds the shallow socket of the shoulder joint (glenoid). This ring is called the labrum. The glenoid labrum increases the depth of the socket making the shoulder joint more stable. A tough, but thin elastic tissue (capsule) further surrounds the shoulder like a bag. The capsule contains a series of ligaments or bands, which connect the humerus to the glenoid.

The most common cause for shoulder dislocation is a forceful injury like falling on an outstretched hand (sports injuries, falls) or a hard blow to the shoulder (a cricket injury or a road traffic accident). This is called a traumatic dislocation.

The force that causes this injury can cause the labrum to be torn from the socket making it shallow. This lesion is known as a Bankart’s lesion and it can lead to further episodes of subluxation or dislocation. Sometimes a relatively minor force may dislocate the shoulder for the first time and the patient may feel a pop as it reduces by itself. This will occur in people who have normal but lax joints. This is referred to as an atraumatic dislocation.
A very small group of patients can dislocate their shoulders without any trauma. These type of dislocations / subluxations occur because of abnormal working of the muscles around the shoulder. Such a condition is referred to as ‘positional instability of the shoulder’.
What are the symptoms and how is it diagnosed?
When the shoulder dislocates the first time after an injury, the patient will immediately complain of pain, deformity and weakness in the shoulder. The patient may develop bruising and complain of numbness or tingling if any of the nerves around the shoulder have stretched.
The symptoms of shoulder instability will range from obvious repeated dislocations, to just pain with certain activities or shoulder positions. Patients
may complain of clicking or popping of the shoulder, the arm suddenly ‘feeling dead’ or the shoulder been generally weak.

Will further tests or investigations be needed?
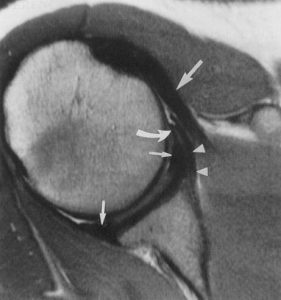
After appropriate clinical assessment, an x-ray of the shoulder is recommended. When the shoulder is dislocated the first time an x-ray will reveal any broken bone. In some situations after the first injury, or if the first injury progresses to instability, a MR Arthrogram is advised. A dye is injected into the shoulder and a magnetic field is used to create cross sectional images of the shoulder.
Sometimes a CT scan may be recommended to assess the bony defects.
Electrical tests may also be necessary if the patient has tingling, numbness or an altered sensation, to assess for any nerve damage.

What is the treatment?
1. After the first dislocation the shoulder will need to be reduced usually in the Accident & Emergency department. This will be carried out using a
muscle relaxant, sedative or rarely a general anaesthetic. Following reduction of the shoulder you will be put in a sling or external brace for a period of time. Physiotherapy is not always needed but may be advised.
2. If the patient goes on to develop shoulder instability, further investigations and treatment may be necessary. Further treatment will depend on the type of instability and the kind of soft tissue or bony injuries.
3. Physiotherapy is the initial line of management in patients who have developed atraumatic type shoulder instability, due to muscle imbalance or abnormal patterns of muscle activity. Some of these cases may not respond to physiotherapy and may need surgical intervention.
4. Surgery is the treatment of choice in patients with traumatic shoulder instability. These patients will demonstrate soft tissue injuries (Bankart’s lesion) or bony defects on the MR Arthrogram. Physiotherapy is unlikely to help in such situations. The aim of surgery is to reconstruct the torn labrum or capsule.
If there is a bony defect it will have to be filled. The surgery is most often done arthroscopically (key hole surgery) in our centre although open surgery may be needed depending upon patient factors.
Arthroscopic (keyhole) stabilisation surgery: About 3-4 small incisions of 5mm each are needed. A telescope is passed into the shoulder through one of these incisions and special surgical instruments are passed through the other incisions to reconstruct the labrum and capsule. The advantage of keyhole surgery is that it is less traumatic and so recovery is quicker. It is usually carried out as a day procedure. Loss of movement of the shoulder is rare after arthroscopic repair.


Open surgery for bony defects: If there is a significant bone loss, keyhole
surgery is not advised. In such circumstances an open
operation (Laterjet Procedure) is performed. This procedure involves transfer of a small bone (tip of corocoid process) with its muscle attachments, to the front of the shoulder socket. The transferred bone is fixed with 1or 2 screws.
What happens if it is not treated?
If the first dislocation occurs in an adolescent there is nearly a 100% chance that the shoulder will dislocate again. Between the ages of 13-18 years there is nearly a 70% chance the shoulder will dislocate again. The younger the person, the higher the chance of re-dislocation.
If the above conditions are not treated it is likely that the symptoms will persist. It may be that the shoulder will become less troublesome if activities
that cause the problems are stopped. It is possible that an unstable shoulder may cause arthritis in the long term but there are no convincing long term studies that conclude this.
What is the success of surgical treatment?
Surgical treatment for traumatic shoulder instability, when the shoulder repeatedly dislocates forward, has a more than 90% success rate.
What are the complications of surgical treatment?
1. Infection of the wound is possible and can usually be successfully treated with antibiotics.
2. Loss of movement is possible especially after open surgery.
3. Damage to the nerve or blood vessels is possible.
4. The operation may fail in about 5-8 % of the patients.
5. If the repair is too tight, osteoarthritis of the shoulder may result in the long term.
6. When bone is transferred to address the bony defects (Latarjet procedure), the bone may not heal.
7. Any surgical intervention has the risk of developing complications that are unpredicted. These complications may have the potential to leave the patient worse than before surgery.
Is there anything I can do to improve the outcome?
Keep the wounds dry and clean until they have healed.
It is important to remember that during the operation, ligaments were reconstructed. The shoulder will be protected in a sling after the operation and the physiotherapist will supervise rehabilitation of the shoulder after the operation. It is very important that the instructions are followed.
When can I do various activities?
Return to work depends on many factors including the nature of the job and hand dominance. Generally you will be able to return to a desk job within 4 weeks of the operation and perform reasonable tasks with the limb within 4-6 weeks. You will be unable to drive for a period of 6-8 weeks and activities like
cricket and racquet sports are best avoided for at least 3 months. Contact sports can be resumed after 4-6 months.
These recommendations will vary from patient to patient.

